
Scientifica's picks of the best neuroscience research from April 2021
Scientifica's selection of the top neuroscience stories from April includes a hydrogel that acts as a 'brain glue' to treat traumatic brain injury, increased understanding of how the intoxicating effects of alcohol arise and the identification of four subtypes of Alzheimer's disease.
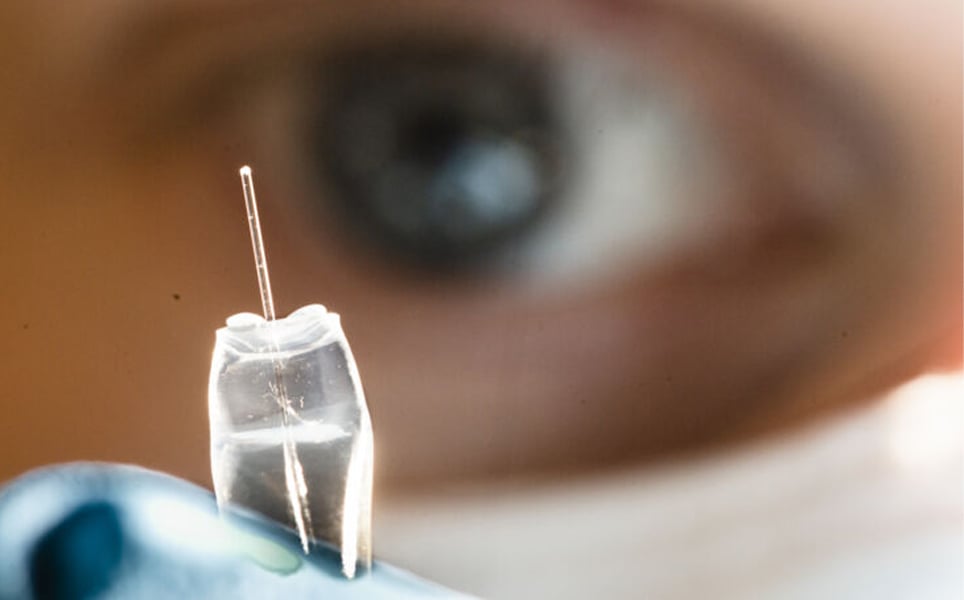
1. First human use of high-bandwidth wireless brain-computer interface
In a clinical trial conducted by BrainGate researchers, a wireless transmitter that is capable of delivering high-bandwidth neural signals has been used in humans for the first time.
The brain-computer interface (BCI) used in the trial is the first intracortical BCI that has no external wires, and is instead connected to an external wireless transmitter. Trialled in patients with tetraplegia, the BCI was able to transmit brain signals at single-neuron resolution without physically tethering the user to a decoding system.
A small transmitter replaces the external wires; this is placed on top of the user’s head, and connects to an electrode array in the motor cortex.
The study showed that the wireless system was able to transmit signals as effectively as wired BCIs. This is an important step towards the development of afully implantable intracortical system that will enable paralysed patients to move again.

Wireless BCI
2. ‘Brain glue’ helps repair circuitry in severe TBI
A hydrogel has been used to treat traumatic brain injury (TBI) by researchers at the University of Georgia Regenerative Biosciences Center.
The hydrogel was created in 2017, and is designed to mimic the structure and function of the naturally occurring network of sugars that support brain cells. The study demonstrated that the hydrogel, which acts as a ‘brain glue’, protects against loss of brain tissue following severe injury, and may also promote functional neural repair.
More here
3. A 3D structure reveals how a unique molecular switch in our brain causes us to feel full
Researchers from the Weizmann Institute of Science, Queen Mary University of London and the Hebrew University of Jerusalem have elucidated the mechanism of action of the melanocortin receptor 4 (MC4), which is found in the hypothalamus of the brain and is a master switch for hunger.
When the MC4 receptor is activated, it causes us to feel full. However, when our energy levels drop, the MC4 receptor is switched off, sending out signals that make us feel hungry. Certain mutations cause the MC4 receptor to remain in its deactivated state, making people feel constantly hungry.
Setmelanotide is an anti-obesity drug that targets the MC4 receptor. Using cryogenic electron microscopy, the team of researchers were able to elucidate the 3D structure of the MC4 receptor, which showed that setmelanotide binds to the receptor with more potency than the natural satiety hormone, activating it to cause feelings of being full. A calcium ion also binds, enhancing the binding of the drug to the receptor. The researchers also found out how mutations in the MC4 receptor can interfere with this signalling, preventing activation, leading to permanent feelings of hunger and obesity.
This enhanced understanding of the structure of the MC4 receptor could lead to the development of drugs that bind to the MC4 only, reducing side effects caused by interactions with other receptors and improving treatments for obesity.
Switching off hunger in the brain
4. An ion pump to deliver chemotherapy agents to the brain
Cell culture experiments by scientists at Linköping University and the Medical University of Graz have demonstrated for the first time that an ion pump could more accurately deliver chemotherapy drugs to malignant brain tumours.
Cells used in the research were from glioblastoma, the most common and aggressive type of brain cancer. There are only a few drugs currently available that can pass through the blood-brain barrier to enter the brain and attack cancer cells. The team used an implanted ion pump to enable a chemotherapy drug, gemcitabine, to pass through the blood-brain barrier. In normal circumstances, this drug is unable to cross the blood-brain barrier, and therefore cannot be used to treat brain cancer.
Existing treatments for glioblastoma harm both cancer and neuronal cells. However, as gemcitabine works by disrupting the cell division process in rapidly growing tumours, and brain cells do not generally undergo cell division, this drug would be a much more effective way to specifically target cancer cells in the brain. Using the ion pump to transport this drug into the brain, cancer cells will be attacked whilst neuronal cells would remain healthy.
Pumping chemotherapy into the brain
5. Study shows smartphone app can identify autism symptoms in toddlers
A smartphone app has successfully been used to identify a main symptom of autism in young children, and could one day be used as a screening tool, researchers at Duke University have found.
The app uses computer vision and machine learning to track the eye gaze patterns of toddlers while they watch short moves on an iPhone or iPad, and determine if they look at the human or objects more often.
By determining whether a child’s preference is to look at objects or people, their likelihood of being diagnosed with autism can be assessed, with toddlers who focus more on objects being more likely to be later diagnosed with autism.
Using the app takes less than 10 minutes, and only requires an iPhone or iPad, making it easily accessible and ideal for use both in the clinic and at home. It is hoped that this technology will provide and easier and more accessible way to screen for autism, enabling earlier intervention.
Improved screening for autism
6. New study showing how the brain retrieves facts and personal experiences may help people with memory disorders
Researchers at the University of York have identified a shared set of systems in the brain that may play a vital role in the retrieval of weak memories. These findings may enable us to better understand and treat memory disorders.
The brain’s long-term memory storage is categorised into factual memory and memory of personal experiences. Previous research has shown that these two memory stores are located in two separate brain regions. However, using functional magnetic resonance imaging, this study demonstrated that a shared brain mechanism is required to retrieve weak memories from these two memory systems. It is thought that this shared control over our memories enables us to retrieve relevant memories to make sense of the world around us and adapt as our goals or circumstances change.
Improved insight into memory
7. Researchers map brain regions responsible for intoxicating effects of alcohol
The intoxicating effects of drinking too much alcohol – slurred speech, poor coordination and sedative effects – may be caused by the breakdown of alcohol products produced in the brain, rather than in the liver.
This research, by the University of Maryland School of Medicine (UMSOM) and the National Institute on Alcohol Abuse and Alcoholism, contrasts to previous findings and provides potential new treatments for alcohol abuse.
The researchers used magnetic resonance imaging to measure the distribution of the acetaldehyde dehydrogenase 2 (ALDH2) enzyme in the brain. The ALDH2 enzyme breaks down acetaldehyde, a bi-product produced when the alcohol dehydrogenase enzyme breaks down alcohol in the liver. This breakdown of acetaldehyde forms acetate, which is a much less toxic substance.
The results showed that the ALDH2 enzyme was responsible for the breakdown of acetaldehyde into acetate in the brain, and alcohol-induced cellular and behavioural effects were found in specific regions of the brain where this enzyme was expressed. Acetate was found to interact with GABA in the brain, which is known to decrease nervous system activity. This decreased activity could lead to drowsiness, impaired coordination, and reduced inhibition.
Next, the researchers will investigate whether alcohol metabolism is regulated in the brain. If this is the case, potential new targets for treating alcohol use disorder could be identified.

Potential new target for alcohol abuse
8. Research breakthrough in understanding how neural systems process and store information
Using a combination of sophisticated mathematical modelling and lab-based experiments, scientists from the University of Exeter and the University of Auckland have gained a better understand of how neural systems encode information.
The researchers discovered that a single neuron can select between different patterns, depending on the properties of a stimulus. This response of a single neuron to a stimulus is a first step in understanding how groups of neurons respond to external stimuli.
It is hoped that this will lead to a better understanding how neural networks form memories, and could also lead to improved insights into the causes of conditions that affect memory, such as dementia.
Learn more
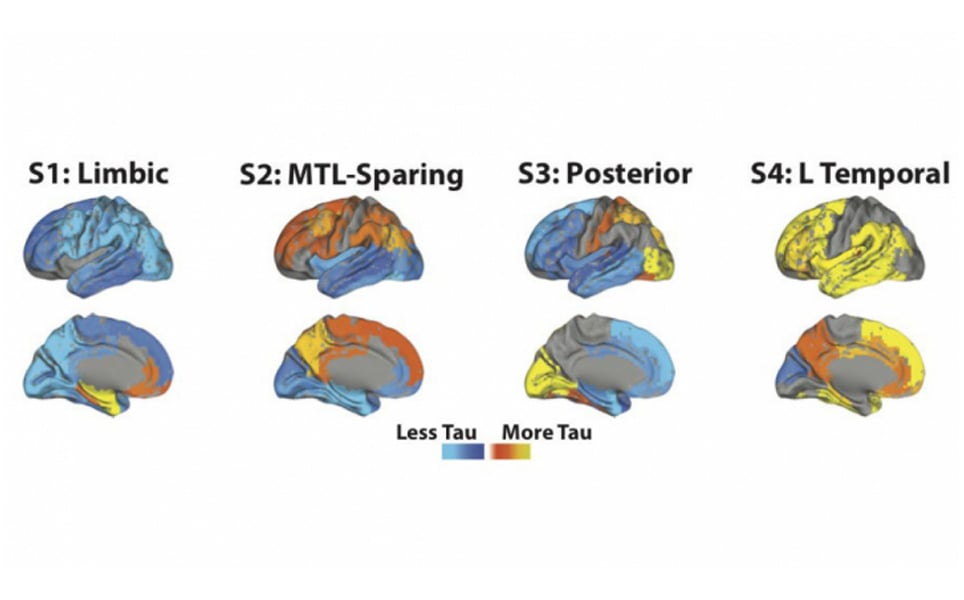
9. Alzheimer's disease is composed of four distinct subtypes
A collaborative study involving researchers from Lund University and McGill University has identified four subtypes of Alzheimer’s disease, which are distinguished by the pattern of how the tau protein spreads in the brain.
The study applied an algorithm to analyse long-term data from a large and diverse population of pre-symptomatic Alzheimer’s patients, those with mild memory difficulties and patients with fully developed Alzheimer’s disease. Machine learning was used to distinguish the subtypes, leading to the identification of four clear patterns of tau pathology.
The results show that Alzheimer’s is a diverse disease, with varying tau pathology. Different regions of the brain are affected differently in each of the four subtypes that have been identified, which explains why different patients can have different symptoms. The different subtypes could also respond to different treatments differently.
The diversity of Alzheimer's disease
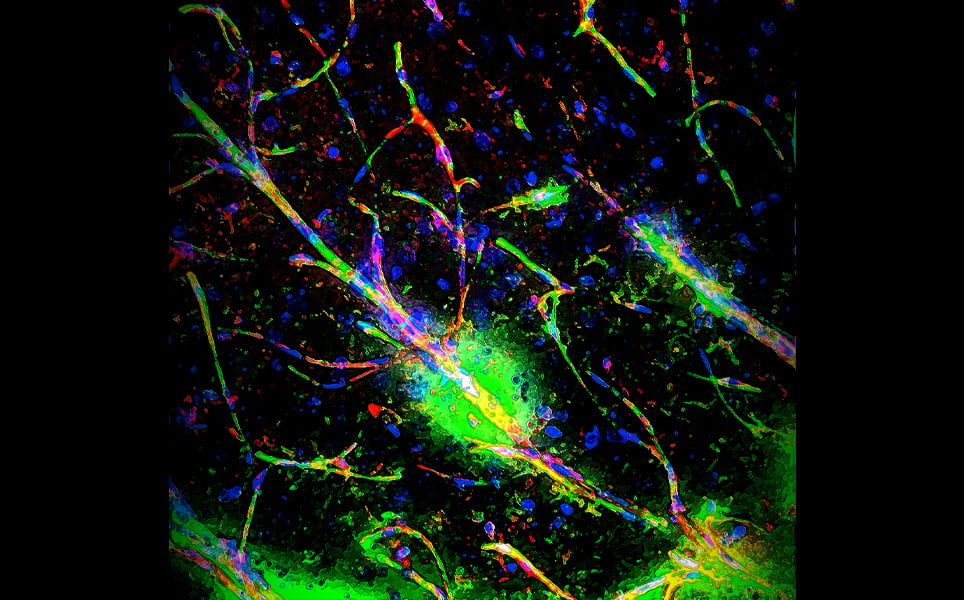
10. The immune link between a leaky blood-brain barrier and schizophrenia
Research by the University of Pennsylvania and the Children’s Hospital of Philadelphia suggests that a leaky blood-brain barrier, that allows immune cells to enter the brain, may be responsible for some of the symptoms of schizophrenia and other neuropsychiatric conditions.
Usually, the blood-brain barrier prevents immune cells, which could cause unwanted inflammation, from entering the brain. If the blood-brain barrier ‘leaks’, allowing some of these cells to enter, it could cause inflammation.
The team studied 22q11.2 deletion syndrome (22qDS), a rare condition where people are born missing a small part of their DNA from chromosome 22. With around a quarter of people with 22qDS developing schizophrenia, understanding this condition could provide insights into schizophrenia. Through extensive studies using stem cells, mice and post-mortem tissue, the researchers found that 22qDS compromises the blood-brain barrier, enabling more immune cells and pro-inflammatory molecules to cross it.
This work adds to the growing evidence that schizophrenia and other neuropsychiatric conditions may be party caused by neuroinflammation. Future work will investigate what causes the blood-brain barrier’s increased permeability, with a focus on astrocytes, which usually enhance barrier function.
Leaky blood-brain barrier and schizophrenia
Banner image credit: Jorge Iván Alvarez

)