
Scientifica’s picks of must-read neuroscience stories from October 2018
Must-read neuroscience stories from October 2018 include identification of the brain’s ‘sleep switch’, successful transplantation of human brain cells into a mouse brain and human retinas grown from scratch in the lab. We hope you find these interesting!
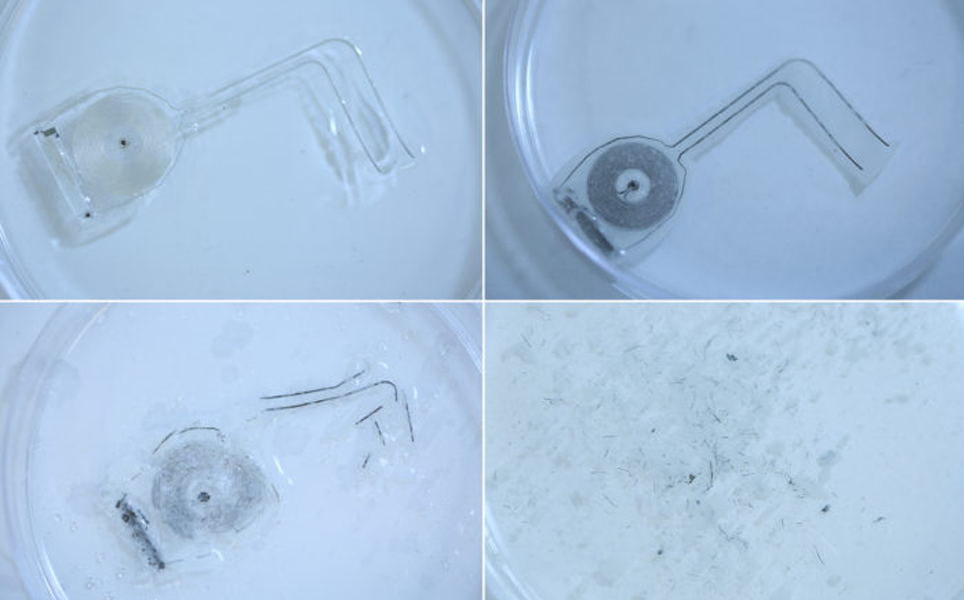
1. Implantable, biodegradable devices speed nerve regeneration in rats
Scientists at Washington University School of Medicine in St. Louis and Northwestern University have developed an implantable, biodegradable device that helps nerve regeneration in rats.
The device delivers pulses of electricity to damaged peripheral nerves at regular intervals. This helped the rats regrow nerves in their legs and gain nerve function and muscle strength faster. If successful in humans, the device could offer a new treatment for peripheral nerve injury.
Read more
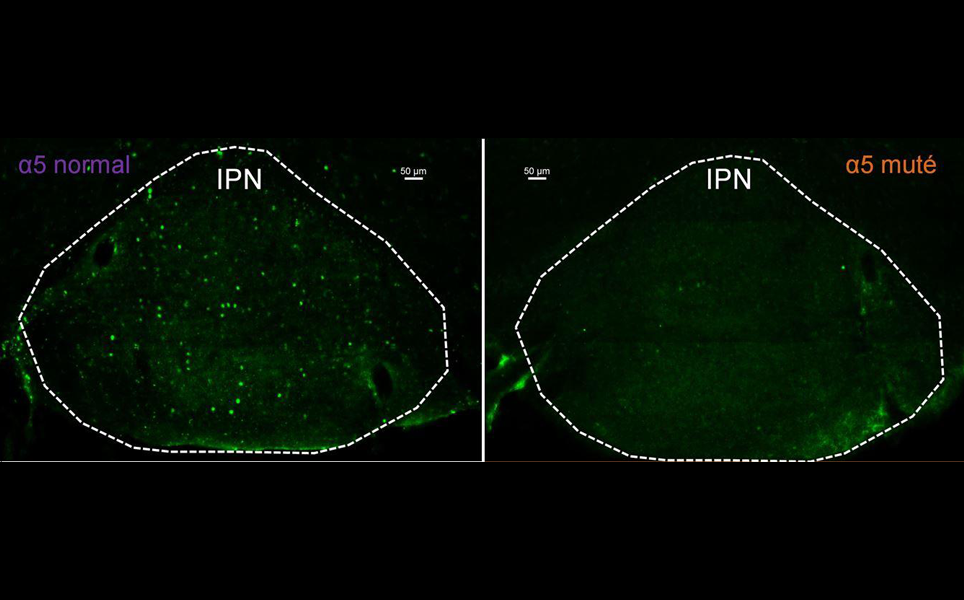
2. Smoking cessation: a genetic mutation involved in relapse
Researchers at the Institut Pasteur, Sorbonne University and Inserm have shown that a genetic mutation, already known to be involved in nicotine sensitivity, is also involved in relapse behaviour.
The researchers found that a mutation present in the gene that encodes the α5 subunit of nicotinic receptors is associated with a significant increase in the risk of smoking. They also identified that the mutation caused higher nicotine consumption at higher doses and greater relapse after cessation. The greater relapse was linked to reduced activation of neurons in the interpeduncular nucleus, which has the highest concentration of nicotinic receptor α5 subunits.
The findings suggest that drugs that increase the activity of nicotinic receptors containing the α5 subunit could reduce tobacco use and risk of relapse after withdrawal.
Reducing relapse
3. AI could predict cognitive decline leading to Alzheimer’s disease in the next 5 years
A team of scientists have trained an artificial intelligence algorithm to accurately predict an individual’s cognitive decline leading to Alzheimer’s in the next five years.
The algorithm, designed by scientists from the Douglas Mental Health University Institute, the University of Toronto and the Centre for Addiction and Mental Health, learns signatures from magnetic resonance imaging (MRI), genetics, and clinical data to help predict if an individual’s cognition is likely to decline in the next five years.
AI Alzheimer's Algorithm
4. Out like a light: researchers ID brain's 'sleep switch'
Researchers at the Beth Israel Deaconess Medical Center (BIDMC) have discovered that a set of neurons in the ventrolateral preoptic nucleus of the hypothalamus are essential to normal sleep.
The VLPO neurons, when activated, stimulate sleep. Activating these neurons also caused a fall in body temperature; body temperature does fall slightly during sleep. Prolonged activation of the VLPO neurons caused the mice's body temperatures to fall by five or six degrees Celsius. The team proposed that the continued firing of these neurons could cause the prolonged sleep and drop in body temperature that occurs in animals that hibernate.
Switching on sleep
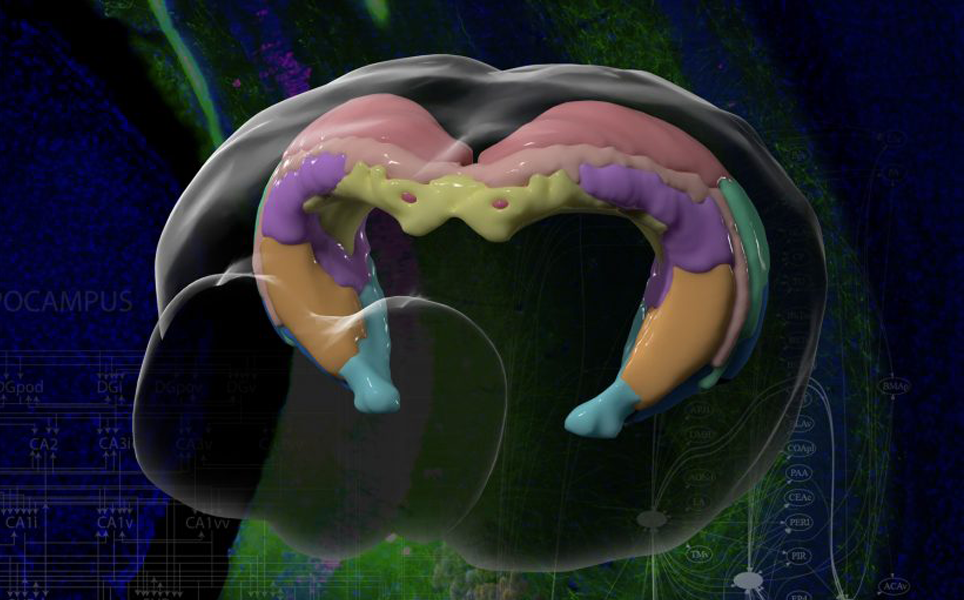
5. USC scientists map brain region linked to Alzheimer’s and other diseases
Scientists at USC have created the most detailed atlas of the hippocampus to date, showing structures and nerve connections in detail.
The researchers used fluorescent tracers and 3D animation to show structures, connections and functions of different regions. It is part of the Mouse Connectome Project at USC, which aims to map all the connections in the brain. The atlas will enable scientists to better understand the hippocampus and how diseases are caused by its degeneration.
Memory region map
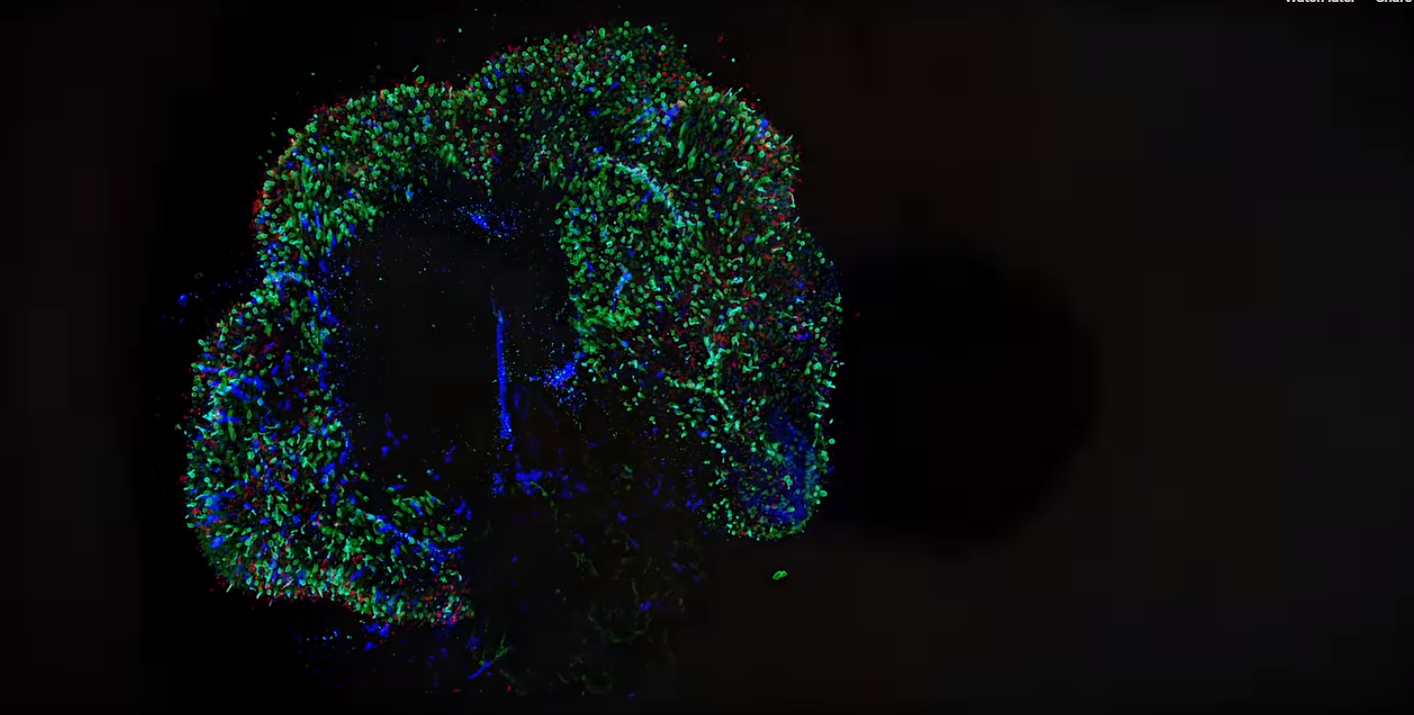
6. Human brain cell transplant offers insights into neurological conditions
Scientists at Imperial College London and the University of Cambridge have, for the first time, successfully transplanted human brain cells into a mouse brain.
The researchers were able to watch how the brain cells grew and made connections with each other. The team used the method to model Down’s Syndrome, and hope the technique could be used to study a variety of brain conditions.
Find out more
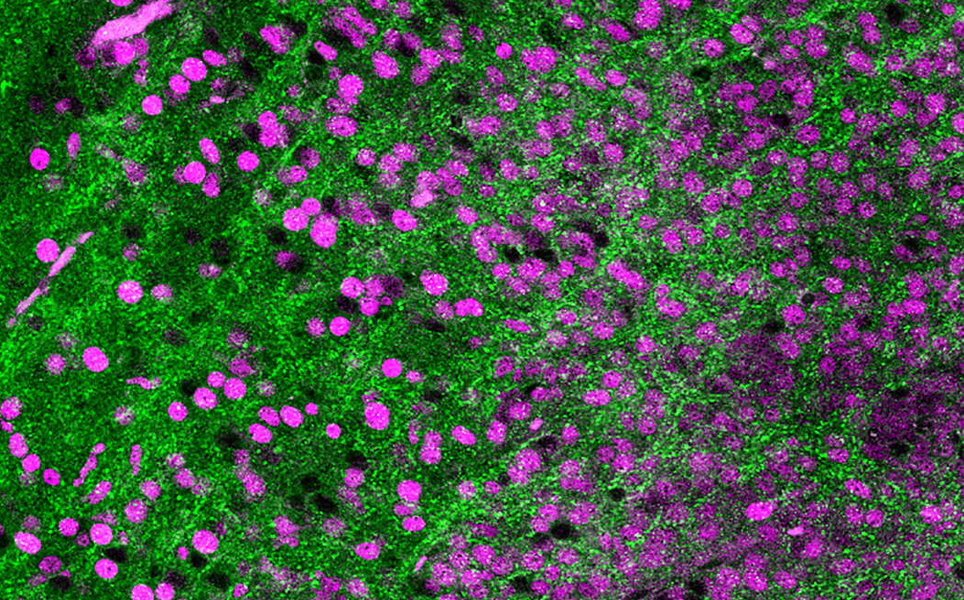
7. Human retinas grown in a dish explain how colour vision develops
Scientists at Johns Hopkins University have grown human retinas from scratch to see how the cone photoreceptors that enable people to see in colour develop.
Stem cells were used to grow the human retina tissue. As the cells grew into retina tissue, it was seen that blue-detecting cells developed first, then red- then green-detecting cells. The molecular switch that turned on the growth of the cells was thyroid hormone, which was controlled by the eye itself, rather than the thyroid gland. The team found that thyroid hormone is essential or creating red-green cones.
The organoids are hoped to be used in the future to investigate vision disorders and macular degeneration.
Seeing colour
8. Tufts scientists grow functioning human neural networks in 3D from stem cells
Scientists have developed 3D brain tissue models that mimic structural and functional features of the brain.
The models, produced by researchers at Tufts University, consist of a 3D matrix of collagen and silk protein, as well as human induced pluripotent stem cells (iPSCs) that are engineered to differentiate into different neuronal cell types. Cells from patients with brain disorders, including Alzheimer’s and Parkinson’s disease, can be incorporated into the models to enable disease mechanisms and potential treatments to be investigated.
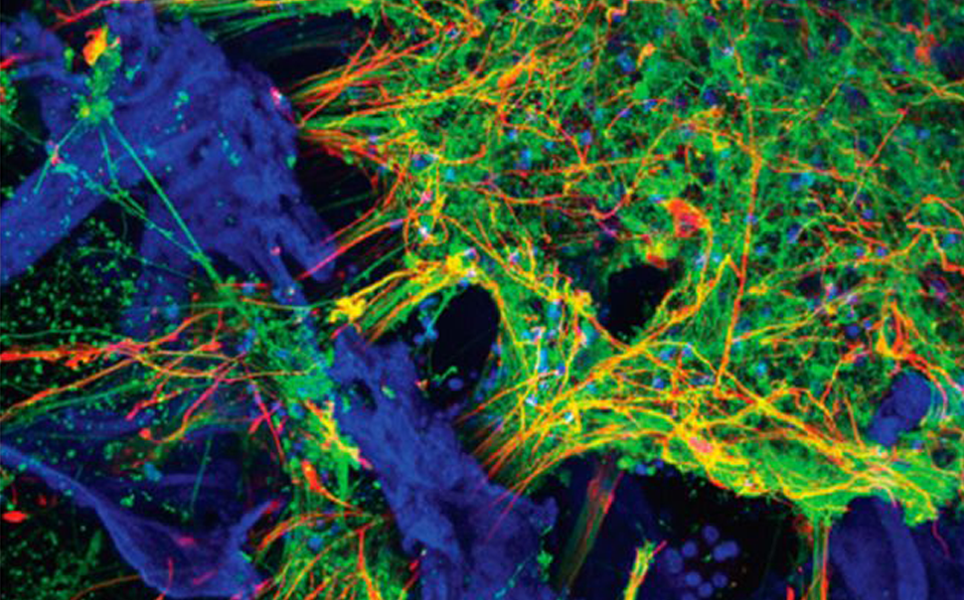
Modelling the brain
9. Study points to new method to deliver drugs to the brain
Researchers have discovered that the glymphatic system could be used to more effectively deliver drugs to the brain. The glymphatic system connects to the brain’s blood vessels and removes waste by pumping cerebral spinal fluid (CSF) through the brain’s tissue.
In mouse experiments, the University of Rochester Medical Center researchers administered antibodies into the CSF, then injected the mice with hypertonic saline. The saline caused an ion imbalance which pulled CSF out of the brain. New CSF was delivered by the glymphatic system to replace this, which contained the antibodies. This meant that the glymphatic system transported the antibodies into the brain tissue.
This method could potentially be used to deliver large proteins and small molecule drugs to the brain, which are usually blocked by the blood-brain barrier.
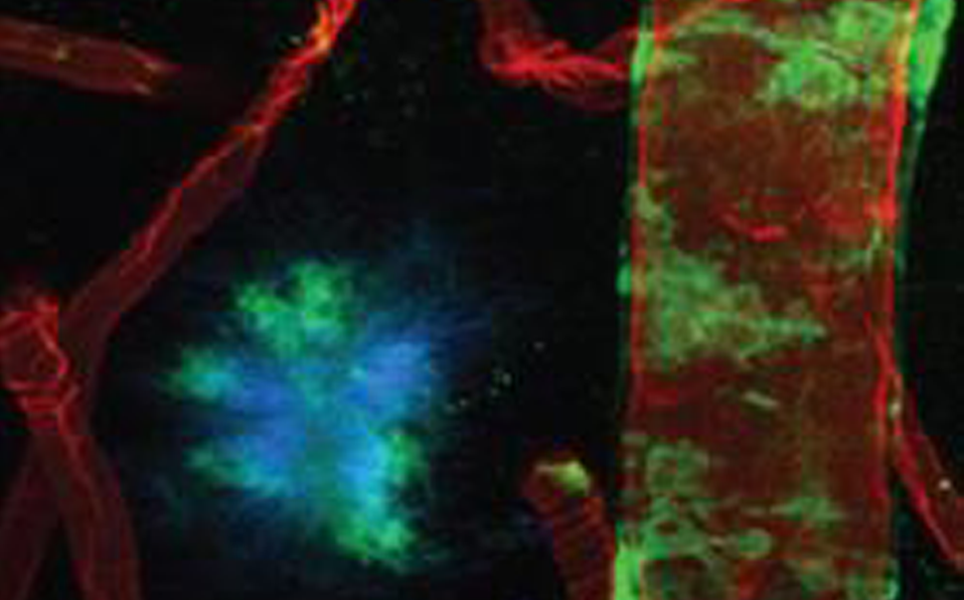
Transporting to the brain
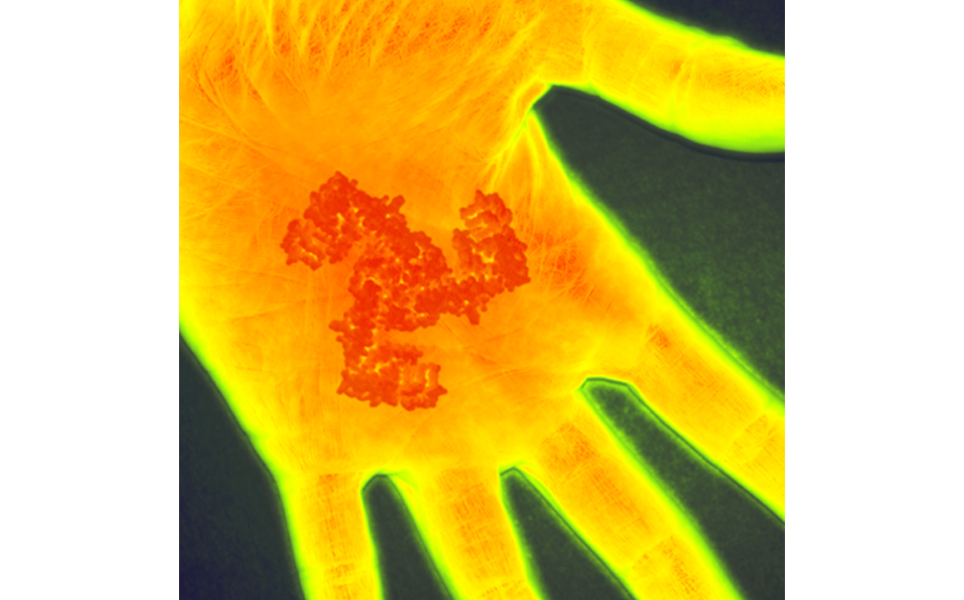
10. Study identifies gene that makes gentle touch feel painful after injury
Two NIH-funded studies have found that the PIEZO2 gene may play an essential role in the nervous system’s reaction to injury and inflammation. The researchers believe it has a role in tactile allodynia, where gentle touch feels painful due to injury.
This offers a potential new target for relieving pain caused by skin injuries, including cuts and burns. If PIEZO2 could be specifically targeted at the site of injury, pain could be relieved without causing numbing to other areas of the body.
PIEZO2 pain
Please send all hippocampus atlases, biodegradable devices, nicotinic receptors, comments and suggestions to [email protected]
Take a look at the top neuroscience stories from previous months...
Sign up to receive our latest news
Find out about Scientifica's latest product releases, company news, and developments through a range of news articles, customer interviews and product demonstration videos.

)